Overview:
- Open conversations break stigma around hormonal health
- Hormonal literacy and access to gynaecological care are essential
- Gender bias continues to affect diagnosis and treatment
- Hormonal imbalances impact fertility and life planning
Women’s hormonal health in India remains stuck between silence and stigma, low hormone literacy and poor gynaecological care access. The lack of literacy continues to delay the actual diagnosis and treatment of women.
Women grow up managing hormonal discomfort but rarely ever know why their bodies change the way they do. Women’s hormones regulate mood, sleep, fertility, body-weight, energy and emotional levels – yet any conversation around it remains under wraps.
Lack of dialogue about women’s hormonal health has established a severe gap in hormone literacy. This lack affects physical health, fertility choices, career participation and overall well-being of a woman. Women’s health in India continues to suffer not because of lack of solutions, but due to lack of awareness.
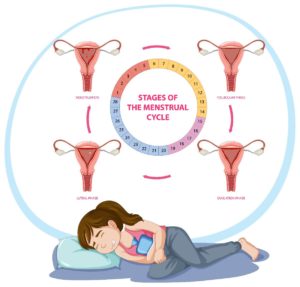
Image Credit- Freepik
Cultural Taboos and the Normalization of Suffering
This cultural silence has normalised long term suffering. When symptoms become regular, women often hesitate while seeking medical help.
Medical conditions such as PCOS, thyroid disorders and endometriosis often remain unattended and undiagnosed for years. By the time a woman decides to seek medical care, the complications have already progressed.
From the first day of period to menopause, hormonal changes shape the life of a woman. Yet in so many households, conversations about menstruation and reproductive health still remain a taboo.
Girls are warned about rules but they are rarely ever explained the biological reasons behind a period. Pain, irregular cycles, fatigue, mood swings are often dismissed as the natural part of being a woman.
Weak Sex Education and the Crisis of Hormone Literacy
School education shapes young minds about health awareness, yet sex-education in India remains inconsistent. Students might be learning about the reproductive anatomy of plants and animals in classrooms.
However, they rarely understand how hormones influence real life health changes-this creates knowledge without clarity.
Poor hormone education creates young women who cannot distinguish between normal changes and warning signs. Women only visit doctors and seek much needed medical attention when it disrupts their daily routine.
When education fails to create awareness, the silence continues throughout generations, passing down coping mechanisms instead of scientific reasons.
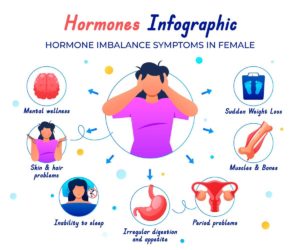
Image Credit- Freepik
Gender Bias and Gaps in Healthcare Access
When women decide to seek medical care, they often face invisible cultural and gender barriers within the healthcare system. A woman’s pain is normalized, minimized or attributed to emotional stress. Hormonal symptoms are dismissed as stress or lifestyle imbalance without proper due-diligence.
A man with similar complaints of hormone imbalance receives faster and more aggressive investigations. This reflects deep rooted gender bias in our society and even in clinical decision making.
Limited and restricted access to gynaecological care worsens these outcomes outside metropolitan cities. This limited access leaves women in rural and semi-urban areas reliant on congested government hospitals. Many women see medical attention as a last resort rather than a routine part of health maintenance.
Emotional and Mental Health Consequences
Women’s hormones influence emotional well-being, anxiety levels and stress mechanisms. A lack of hormonal literacy creates a source of shame instead of a signal for care and medical attention.
In India, women are prescribed psychiatric medication without any proper diagnosis or hormone check-up. While mental health support is crucial, an untreated hormonal imbalance continues to intensify the symptoms beneath the surface.
An open conversation on hormonal health in India can change this dynamic, when biological reasons are understood, self blame lessens.
Workplace Participation and Productivity
Hormonal disorders affect energy levels, sleep and physical endurance. Women experience unmanaged symptoms, and often push themselves through workdays without any support or guidance.
Workplaces rarely offer structured policies or rules addressing menstrual health, fertility treatment or hormonal imbalance disorders. A menstrual leave policy remains controversial rather than normalised in India. Every woman deserves a menstrual leave whether working in an office,or at home.
Improved hormonal literacy understanding benefits not only a woman’s health but also organisational productivity. When women are able to receive timely medical attention followed by treatments, burnout reduces and stability improves.
Fertility Decisions and Long Term Life Planning
Hormonal changes play an important role in ovulation, egg quality and overall reproductive health of a woman. Many women only discover these issues when they begin family planning. The emotional weight of fertility issues brings shame and embarrassment due to delayed diagnosis.
Early diagnosis and accessible treatment can transform this experience. When hormonal literacy is available, women make well-informed decisions about family planning, egg freezing and long term health goals.

Image Credit- Freepik
The Need for Open and Science Led Conversations
Silenced conversations give power to myths, science takes that power back by explaining biological reasons. When conversations surrounding hormones, sex-ed, pregnancy moves into homes, classrooms, media-the fear naturally loses its grip.
Doctors, teachers, educators must work as a bridge to complete the gap between science and daily life. Digital platforms must actively spread hormonal literacy at large.
Community based medical services can expand gynaecological care access in rural regions.
Conclusion
Women’s hormonal health in India has remained neglected for far too long, under the constant weight of silence and stigma. Poor hormonal literacy and weak medical care access delays a timely diagnosis which can help avoid deep suffering.
Open conversations backed by scientific and biological reasons can change the traditional mindset and create a better place for women.
When understanding replaces shame and embarrassment, health becomes a priority rather than a silent burden.


